Do you spend long hours standing at work? Whether you work in sales, retail, or hospitality, standing for extended periods can take a toll on your legs. Have you noticed your leg veins becoming more prominent or tender? Do you experience swelling, aching, or skin changes near your ankles?
If so, you might be at risk of developing varicose veins. But don’t worry—there are steps you can take to reduce your risk and improve circulation. In this article, we’ll explain what varicose veins are and share seven practical tips to keep your legs healthy.
Table Of Content
What Are Varicose Veins?
The Physiological Mechanism
Your circulatory system works against gravity to pump blood back to the heart. Tiny valves in your veins open to allow blood flow toward the heart and close to prevent it from flowing backward. When these valves weaken or become damaged, blood can pool in the veins, causing them to stretch, twist, and become varicose veins.
Varicose veins can develop anywhere in the body but are most commonly found in the legs due to prolonged standing or sitting.
Causes of Varicose Veins
Varicose veins result from increased pressure in the veins near the skin’s surface. Long periods of standing or sitting can lead to blood pooling in the legs, increasing pressure and making veins more susceptible to damage.
Risk Factors
Some individuals may be more prone to varicose veins due to genetic or lifestyle factors. Common risk factors include:
- Family history – Varicose veins can run in families.
- Excess weight – Increased body weight places added pressure on the veins.
- Age – The risk increases with age as vein walls lose elasticity.
- Smoking – This weakens blood vessels and affects circulation.
Symptoms of Varicose Veins
While varicose veins are not always a serious medical condition, they can cause discomfort and affect your daily life. Symptoms may include:
- Skin color changes
- Leg sores
- Rashes
- A feeling of heaviness, burning, or aching in the legs
What Are Spider Veins?
Spider veins are a milder form of varicose veins. They are smaller, often appearing as red or blue web-like patterns on the legs or face. Though usually harmless, they may indicate underlying circulation issues.
7 Tips to Lower Your Risk of Varicose Veins
- Move Frequently – Avoid standing or sitting in one position for too long. Shift your weight, stretch, or take short walks every 30 minutes to keep blood flowing.
- Exercise Regularly – Activities like walking, swimming, and cycling help strengthen leg muscles, improving circulation and vein function.
- Maintain a Healthy Weight – Managing your weight reduces pressure on your veins and improves circulation.
- Avoid Smoking – Smoking weakens veins and can contribute to poor circulation, increasing your risk of varicose veins.
- Elevate Your Legs – Whenever possible, raise your legs above heart level for a few minutes to improve blood flow and reduce swelling.
- Wear Compression Stockings – These help support blood flow and prevent veins from stretching excessively.
How Are Varicose Veins Diagnosed?
If you experience symptoms of varicose veins, it’s best to seek professional advice. A physiotherapist or doctor may conduct a physical exam and use imaging techniques such as a Duplex ultrasound to assess blood flow and vein structure.
How Can Physiotherapy Help Manage Varicose Veins?
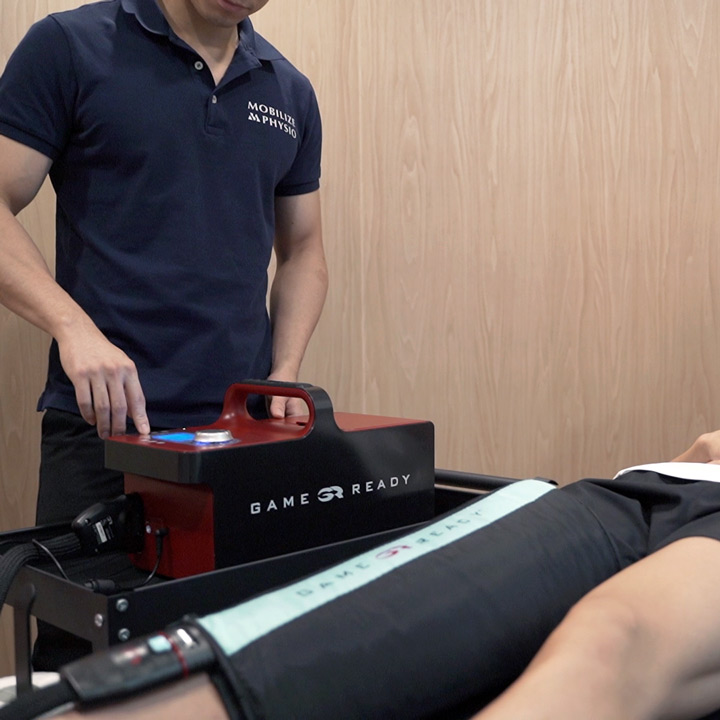
Physiotherapy can be an effective approach to improving circulation and managing varicose vein symptoms. Treatment options include:
- Exercise Therapy – Strengthening and mobility exercises promote blood flow and reduce discomfort.
- Compression Therapy – Specialized stockings help prevent swelling and improve circulation.
- Lifestyle Modifications – Guidance on posture, movement, and activity adjustments to minimize vein strain.
- Pain Management Strategies – Techniques such as massage and elevation can alleviate discomfort.
Take Action for Healthier Legs
If you’re experiencing discomfort from varicose veins, don’t ignore the symptoms. Simple lifestyle changes and physiotherapy can help improve circulation and keep your legs feeling strong and pain-free. Consult a physiotherapist to explore tailored treatment options and maintain your vascular health.






Physiotherapy For Varicose Veins
Mobilize Physio is a physiotherapy center located in Hong Kong. Our team of professional physiotherapists provides high-quality, evidence-based pain treatment. Our services include sports injury treatment, pain management, post-surgery rehabilitation, and posture and body alignment correction.
Every patient is unique, and we believe that every treatment plan should be customized accordingly. Therefore, we focus on one-on-one service to ensure that each patient receives personalized attention and specialized care. Contact us today to learn more about our varicose veins physiotherapy services.
Latest Blog Posts

Conquering Morning Heel Pain in Hong Kong: The Deep Link Between Flat Feet & Plantar Fasciitis

SCHK Marathon Injury Survival Guide: 7 Common Running Injuries, Self-Management & Physiotherapy

SCHK Marathon Injury Prevention Survival Guide: Taping Tips & Physio Secrets for Hong Kong Runners

What Is Shockwave Therapy? A Non-Invasive Solution for Musculoskeletal Pain

ACL Tear: Do You Need Surgery Immediately? Why Prehab & Proper Rehab Matter More Than You Think

Foot Care for Trailwalker & Ultra-Endurance Events: Prevent Injuries, Boost Performance